Bypass Surgery
 Coronary artery bypass surgery is done to provide "detours" around the partially or completely blocked arteries. With a new open "bypass system" the heart can now receive its much needed blood supply.
Coronary artery bypass surgery is done to provide "detours" around the partially or completely blocked arteries. With a new open "bypass system" the heart can now receive its much needed blood supply.
Coronary artery bypass surgery is performed to provide relief of angina, to improve the pumping ability of the heart muscle, to prevent heart attacks, and to reduce the use of heart medications, all of which should improve a patient's quality of life. The indications for surgery vary, depending on each patient's symptoms and findings at the time of heart catheterization. Your surgeon and cardiologist will discuss the reasons for recommending surgery to you.
 The concept of coronary artery bypass surgery is very simple. Healthy arteries or veins are "harvested" to create “bypass grafts” that channel the needed blood flow around the blocked portions of the coronary arteries. The new section of
vessel can come from the mammary artery in your chest, the radial artery in your forearm, or the saphenous vein in your leg. To learn more about vessel harvesting, click here.
The concept of coronary artery bypass surgery is very simple. Healthy arteries or veins are "harvested" to create “bypass grafts” that channel the needed blood flow around the blocked portions of the coronary arteries. The new section of
vessel can come from the mammary artery in your chest, the radial artery in your forearm, or the saphenous vein in your leg. To learn more about vessel harvesting, click here.
The saphenous vein is commonly used for grafts. These veins are used by the surgeon as an alternate vessel to deliver blood to the heart muscle below the point of the blockage. The surgery reroutes the blood flow to supply areas of the heart muscle not receiving enough blood (See Figure 1).
What is Traditional Bypass Surgery?
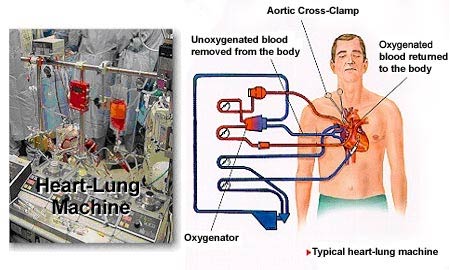
Coronary artery bypass surgery became routine in the late 1950s with the invention of the heart-lung machine. With "traditional" bypass surgery, surgeons use the assistance of the heart-lung machine along with medications to stop the heart so the bypass can be performed on a motionless field. The heart-lung machine is referred to as a "pump" because it continues to mechanically pump oxygen and nutrients to the body during surgery.
Beating Heart Bypass Surgery
Recent advances in surgery and medical devices allow doctors to have less invasive options in the treatment of coronary artery disease (CAD), such as Beating Heart or "Off-Pump" Bypass Surgery. Now individuals who have medical conditions such as diabetes, history of stroke, or poor physical health, can undergo cardiac surgery with lower risk for developing complications. You will want to talk with your doctor to see if Beating Heart Bypass Surgery is an option for you.
Beating Heart vs. Traditional Bypass Surgery
Beating Heart Bypass Surgery is different from traditional bypass surgery because it is performed while your heart is still beating. Your surgeon does not use the heart-lung machine to stop your heart during the procedure. In some cases, the surgeon may still need to use the heart-lung machine during the operation. A perfusionist (a specialist trained to operate the heart-lung machine) may remain on standby during your operation.
With this approach, surgeons can perform multiple bypass grafts on all areas of the heart, including the backside (posterior), at the same time. What this means is, the surgeon can perform a triple (three bypass grafts), quadruple (four bypass grafts) or more through a middle of the chest incision all off-pump
Clinical Benefits of Beating Heart Bypass Surgery
Your physician may choose the beating heart bypass procedure for you because of benefits such as:
- Decreased length of hospital stay1, 2, 3
- Less trauma due to the elimination of the heart-lung machine
- Reduction in need for blood transfusions1, 2, 3
- Fewer cognitive and neurological consequences4, 5 such as stroke6
In addition, a recent study presented in the New England Journal of Medicine showed that patients who are treated with traditional bypass surgery may suffer from lapses in mental acuity that result from brain damage caused by the stopped heart bypass surgery.
Out of 261 patients whose mental acuity diminished after bypass surgery:
- 53% had diminished mental acuity at discharge
- 36% had diminished mental acuity after 6 weeks
- 24% had diminished mental acuity after 6 months
- 42% had diminished mental acuity after 5 years7
Potential benefits of Beating Heart Bypass vs. Traditional Bypass surgery?
When compared to traditional coronary artery bypass procedures that stop the patient's heart and utilize a heart-lung machine, beating heart bypass procedures reduced:
- Transfusion rates by 48%8
- Length of post-operative hospital stay by 40%8
- Hospital costs by 24%8
- Post-operative cognitive dysfunction by 36% at 5 days and 90% at 3 months7
- Understanding your Bypass (CABG) Surgery
- Why Is My Doctor Recommending a CABG?
- Before Your Heart Surgery
- Getting Started (CABG)
- Moving to the Operating Room (CABG)
- General Anesthesia for Heart Bypass Surgery
- What Happens During a CABG?
- Moving to the Intensive Care Unit (CABG)
- Time in the Hospital After Your CABG
- Leaving the Hospital After a CABG
- Leaving the Hospital -- Information for Diabetics
- What Results Can You Expect From a CABG?
- Risks and Complications of Bypass (CABG) Surgery
- How Safe Is a CABG?
- CABG -- Minor Complications
- CABG -- Major Complications
- CABG Complications -- Final Thoughts
- CABG Risks – Infection
- CABG Risks – Stroke
Endoscopic Vessel Harvesting
Many patients are surprised to learn that a bypass operation may actually
include two surgical procedures.
- Primarily, the bypass surgery involves using a healthy blood vessel to "bypass" a damaged or blocked artery in the heart.
- The second procedure is the actual removal of a healthy blood vessel, typically the saphenous vein in the patient's leg, which will be used to construct the bypass.
What is
traditional vessel harvesting?
Traditional vessel
harvesting procedures require a long incision or a series of incisions down
the length of the patient's leg, from the groin to the ankle. The greater
saphenous vein is harvested intact through this large incision. The
harvested vessel is then used as a graft that surgeons sew in place to
bypass the blocked coronary artery.
What is Endoscopic Vessel Harvesting?
Recent advances in technology have made it possible to perform this second procedure in a new, less invasive way, called Endoscopic Vessel Harvesting, or EVH. Rather than make a large incision in the leg of a patient, surgeons can now make small incisions in the patient's leg. Because this new procedure results in less muscle and tissue damage when harvesting the vein graft, this procedure may eliminate many of the complications associated with the former technique. This may offer significant benefits to you.
How is Endoscopic Vessel Harvesting Performed?
An endoscope, a special instrument used to view the inside of a hollow area, is connected to a video camera and inserted through a small incision in the leg. The endoscope is used to view the saphenous vein inside the leg and allows the surgeon to remove the vein with minimal stress to the leg.
What are the patient benefits from Endoscopic Vessel Harvesting?
This new procedure generally results in less muscle and tissue damage and therefore, may reduce the surgical trauma to the patient, reduced wound infections9,10 and decreases the incidence of wound healing complications9,11,12. In other words:
- you should experience less tissue scarring
- your leg wounds should be less painful13
- you should avoid an unsightly scar
- you will be able to concentrate on your cardiac rehabilitation!
In
most cases, the small incision approach can be used successfully. However,
every surgical patient is unique, and your surgical team will recommend the
best procedure for you.
It is important to remember that the goal of any bypass surgery is to
increase coronary artery blood flow. Increased blood flow may:
- Provide relief of angina (pain or tightness in the chest)
- Improve the pumping ability of the heart muscle
- Reduce the risk of heart attacks
Most importantly, the quality of your life should improve.
Endoscopic Radial Artery Harvesting
A bypass operation includes two surgical procedures:- The bypass surgery involves the use of a healthy blood vessel to “bypass” a damaged or blocked artery in the heart.
- The second procedure is the removal of a healthy blood vessel, in this case the radial artery in the patient’s forearm. This vessel will be used to construct the bypass.
Recent advances in technology have made it possible to perform this second procedure in a new way, through endoscopic small incision surgery. This new procedure results in less muscle and tissue damage when removing the vessel graft. This may eliminate many of the complications associated with the former technique, which required a long incision the length of the graft.
In the past a vessel was often removed from the patient’s leg, called a saphenous vein graft. Now surgeons may choose to remove the radial artery in the patient’s forearm instead.
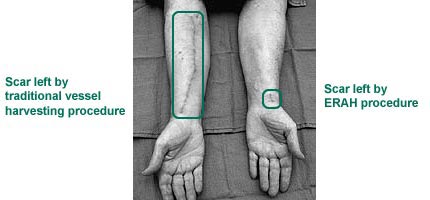
To harvest the radial artery the surgeon makes two small one-inch incisions in the patient’s forearm. One incision is made near the wrist; the other is made near the elbow.
Because radial arteries from the arm are accustomed to higher blood pressure than leg veins, they may prove to be more durable bypass grafts. In the past surgeons had to harvest the radial artery through a long incision from the elbow to the wrist, increasing the potential for complications.
How is Endoscopic Radial Artery Harvesting Performed?
An endoscope, a special instrument used to view the artery, is connected to a video camera and inserted through the small incisions in the forearm. The endoscope allows the surgeon to remove the artery with minimal stress to the forearm.
Patient Benefits from Endoscopic Radial Artery Harvesting
The potential benefits from this procedure include the following:- The patient should experience less tissue scarring.
- The site of the patient’s incision should be less painful.
- The recovery from surgery should be shorter, allowing the patient to concentrate on cardiac rehabilitation.
In most cases the radial artery can be harvested successfully. However, every patient is unique, and the surgical team will recommend the best procedure for each patient.
It is important to remember that the goal of any bypass surgery is to increase blood flow to the heart’s arteries. Increased blood flow may:- Provide relief from angina (pain or tightness in the chest)
- Improve the pumping ability of the heart muscle
- Reduce the risk of heart attacks
- Most importantly, improve the quality of life
1. van Dijk D et al. Early outcome after off-pump versus on-pump coronary bypass surgery: results from a randomized study. Circulation, 2001 Oct 9;104(15):1761-6.
2. Puskas JD et al. Clinical outcomes, angiographic patency, and resource utilization in 200 consecutive off-pump coronary bypass patients. Annals of Thoracic Surgery, 2001 May, 71(5):1477-83.
3. Puskas JD et al Off-Pump coronary artery bypass grafting provides complete revascularization while reducing myocardial injury, transfusion requirements and length of stay: Prospective randomized comparison of 200 unselected patients having OPCAB Verses conventional CABG. Journal of Thoracic and Cardiovascular Surgery. (in press). Newman, MF et al.; Longitudinal Assessment of Neurocognitive Function After Coronary Artery Bypass Surgery. New England Journal of Medicine, February 8, 2001, 344 (6): 395-402
4. Lee JD et al. Off pump coronary artery bypass reduces neurological and clinical morbidity: A prospective randomized trial. Paper presented the Asia Pacific Scientific Forum, April 23-26, 2002, Honolulu, HI.
5. Stamou SC et al. Stroke after conventional versus minimally invasive coronary artery bypass. Annals of Thoracic Surgery 2002 Aug;74(2):394-9.
6. Puskas JD; Wright CE, Ronson RS; Brown WM; Gott JP; Guyton RA. Clinical Outcomes and Angiographic Patency in 125 Consecutive Off-Pump Coronary Bypass Patients. Heart Surgery Forum 1999; 2(3): 216-221
7. Murkin JM; Boyd WD; Ganapathy S; Adams SJ; Peterson RC; Beating heart surgery: why expect less central nervous system morbidity? Annals of Thoracic Surgery, 1999 Oct, 68(4): 1498-501
8. Puskas JD et al. Comparison of hospital cost for on versus off pump coronary surgery: Results from a randomized trial. Paper presented at the annual meeting of the American Heart Association, November 18, 2002, Chicago, IL.
9. Bitondo JM & Dagett WM. Endoscopic vs. Open Saphenous Vein Harvest: A Comparison of Post-Operative Wound Complications. Annals of Thoracic Surgery, Feb 2002; 73(2):523-8.
10. Carpino PA, et al. Clinical benefits of endoscopic vein harvesting in patients with high risk factors for saphenectomy wound infections undergoing coronary artery bypass grafting. Journal of Thoracic and Cardiovascular Surgery, Jan 2000; 119(1):69-76.
11. Crouch JD, et al. Open versus endoscopic saphenous vein harvesting: Wound complications and vein quality. Annals of Thoracic Surgery, Oct 1999; 68(4):1513-6.
12. Allen KB, et al. Risk factors for leg wound complications following endoscopic versus traditional saphenous vein harvesting. Heart Surgery Forum 2000; 3(4):325-30.
13. Davis Z, et al. Endoscopic vein harvest for coronary artery bypass grafting: technique and outcomes. Journal of Thoracic and Cardiovascular Surgery, Aug 1998; 116(2):228-35.